Low iron feels terrible and it’s something that so many women with struggle with because of our periods, our diets or sometimes it’s just random bad luck. In this blog post I will help you understand what causes low iron but even more importantly – how to rebuild your iron stores and get your energy back.
Getting enough iron can be really tricky even if you are using supplements so make sure you pay special attention to the section on maximizing iron intake where I outline how to get the most from your food and supplements.
What Causes Low Iron
Everyone loses a bit of iron everyday. If you aren’t getting enough iron in your diet, your iron reserves will fall slowly. If they keep falling, you may develop an iron deficiency. If they fall even further, you won’t have enough iron to make red blood cells. This is called iron deficiency anemia.
Iron deficiency is very common for women until we reach menopause because we lose extra iron every month during our periods. If you have regular cycles, your doctor should suggest testing iron whenever you run any other blood tests but, reality is – a lot of the time we need to ask for it to be tested.
Serum ferritin is usually used as the primary test for low iron and, while it’s not clear from the research, many experts suggest the ideal range of serum ferritin is 40 to 70 ng/ml. You’ll see the reference range on your test results runs from about 20 to 200 ng /ml but for health and longevity purposes you may not want it to be too high either.
Having too much iron is associated with accelerated aging, inflammation and many chronic diseases like cardiovascular and neurodegenerative diseases. That’s why it’s important to get tested before you start supplementing with iron.
Reasons for low iron include:
- Insufficient dietary intake of iron (even more likely if you follow a low calorie diet and/or don’t eat meat)
- Consuming too many foods and beverages that block iron absorption
- Heavy periods and/or prolonged periods
- Pregnancy and childbirth
- Digestive system problems that prevent absorption (for example, iron deficiency is very common in people with inflammatory bowel disease)
- Strenuous exercise, excessive sweating or being a runner (because foot strike can cause iron loss)
- Chronic blood loss (for example, from endometriosis or fibroids, which require a great amount of blood).
Symptoms of Iron Deficiency
If you are iron deficient it’s really important to get on top of it because having low iron feels terrible but it can also have some long term, more serious consequences.
Common symptoms of low iron:
- Fatigue
- Lack of energy and motivation
- Inability to focus or brain fog
- Headache or ringing ears
- Shortness of breath
- Nausea
- Pale appearance
- Changes to your heart rate
- Feeling your heart thumping in your head
- Cold hands and feet
- Low body temperature
- Brittle hair and nails
- Depression or anxiety.
Can You Get Enough Iron From Food?
While you may be able to maintain iron stores through diet if you don’t have something like heavy periods or a digestive problem – it’s pretty much impossible to rebuild them from food alone once they are low.
You get two different types of iron from food – heme and non-heme. Heme iron is found in meat, fish and poultry and non-heme iron is found in plants. Your body is better able to absorb and use heme iron than it is non-heme iron. It’s estimated that you absorb 15-35% of heme iron and 2-20% of non-heme iron.
If you don’t eat meat, it’s recommended that you consume twice as much iron since non-heme iron isn’t absorbed as well. Consuming vitamin C with your non-heme iron sources will substantially increase the amount of iron absorbed (and in the next section I have even more tips for you on maximizing your iron intake).
Interestingly, if you are iron deficient you will be more efficient at absorbing iron from all sources as compared to someone with normal iron levels. However, your body isn’t very good at absorbing iron and many other foods block iron absorption which means even if you are consuming the recommended intake of 18mg of iron daily from food sources, you will only absorb a few grams overall throughout your day.
Foods high in iron (approximate values given):
- Lean trimmed beef (100g) = 3mg
- Chicken thigh meat (100g) = 1.3mg
- Oysters (6 medium) = 5mg
- Mussels (100g) = 7mg
- Lentils (1/2 cup cooked) = 3.3mg
- Black beans (1/2 cup cooked) = 1.3mg
- Black-eyed peas (1/2 cup cooked) = 2.15mg
- Fortified protein powders and bars = depends on brand but may have 20-25% of daily intake
Given the small amount of iron in food and the fact that we don’t absorb that much of it, you can understand why it’s easy to start running low. It will also be difficult to rebuild iron stores from food alone because:
- Unless you eat tons of red meat (or things like mussels and oysters) you won’t consume enough iron to rebuild iron stores.
- Many foods that are high in iron (ie. spinach, chocolate) contain compounds that will block iron absorption (ie. oxalates).
- There are many foods and beverages that inhibit iron absorption.
- If you are restricting calories, it will be even more difficult to consume enough iron rich foods.
- Some foods that are high in iron are also high in calories (ie. Dried fruit contains iron but the serving sizes are often 1/2 cup for just over 1g of non-heme iron.).
Maximizing Iron Intake – Get The Most From Your Food & Supplements
Because so many things block iron absorption if you can manage to take your iron supplements on an empty stomach you may absorb more iron. I try to take my supplements at least 45 minutes before eating.
For reasons you’ll read about in the following section, I’m not a fan of using prescription iron pills so I’ve had to work hard to boost my iron levels from a combo of food and gentler iron supplements. Many foods and beverages block iron absorption so supplementation is actually very complicated.
Here are some tips to make sure you get the most from your iron supplements:
- Tea and coffee will substantially block iron absorption. Avoid drinking 1-2 hours before and after an iron-rich meal and iron supplements.
- Dairy and calcium supplements will block iron absorption so avoid them before and after iron-rich meals and iron supplements.
- Magnesium may decrease non-heme iron absorption and absorption from supplements so take magnesium away from iron-rich meals and iron supplements.
- Zinc competes with iron for absorption so take zinc at a different time than iron. Also, supplementing with iron may decrease zinc levels so if you’ve been using supplements for some time, you may want to take a zinc test (readily available on many websites that sell health supplements).
- Since certain minerals compete with iron for absorption and iron can block absorption of other minerals as well, take your multivitamin at a different time than iron supplements. Also do not use a multivitamin that contains iron.
- Substances called phytates, found in grains, beans, seeds and nuts, will reduce iron absorption. You can reduce phytates by soaking your grains overnight and rinsing them several times before cooking but it’s probably wise to consume grains away from your main iron sources. Fermenting and sprouting grains also helps.
- You’ll reduce phytates by eating white rice instead of brown with your iron sources (ie. if you eat beef stir fry, have some white rice).
- Oxalates, found in foods such as spinach, kale, beets, chocolate, and strawberries, can block iron absorption. That’s why spinach, although high in iron, isn’t a good source of iron.
- Ascorbic acid/vitamin C is the most effective enhancer of non-heme iron absorption. Consuming vitamin C supplements or foods high in vitamin C with iron rich meals will increase the amount of iron you absorb and may negate some of the iron inhibition from phytates and oxalates.
- Eating some meat (heme iron) with non-heme iron sources will also increase the absorption of iron from that meal.
- Egg yolks contain a protein called phosvitin that binds iron and renders it unavailable to the body. Consuming an egg with a meal or supplement will substantially reduce the amount of iron absorbed.
- Some research suggests that you should divide your dose of iron throughout the day rather than taking it all at once. This will also help reduce any stomach problems you have from supplements. However some research suggests taking it all in one big dose is better. In my experience, taking it twice seems to work better for me.
Choosing A Good Iron Supplement
Many women report negative effects from taking prescription iron tablets – with main complaints being stomach ache, nausea and constipation. One of the main problems with prescription iron tablets, which usually contain 325mg of ferrous sulfate or fumarate, is the size. Generally, the larger the dose of iron the more side effects you’ll experience.
If you research iron supplements, you’ll quickly find out that they are “toxic” to your body. In fact, my doctor told me this just the other day as he was writing me a prescription for ferrous sulfate (one that I have no intention on filling but it was pointless arguing with him).
So even though your doctor knows that iron is toxic, they still prescribe it in large dose tablets that upset our stomachs. In fact, if you are low in iron, your doctor may tell you that prescription iron is the only way to restore iron levels which isn’t exactly true. Prescription iron might raise iron levels faster than other smaller dose supplements but if it hurts your stomach, you aren’t going to take it regularly. So that’s not going to work anyway.
The first thing to look for in an iron supplement is the amount of elemental iron because this is the amount that’s actually available for absorption. This isn’t necessarily the same as the amount of iron listed clearly on the box. For example, prescription iron will often say 325mg of iron but the elemental iron is usually only 60-100mg.
The recommended daily intake of elemental iron is 150-200mg per day for iron-deficient patients.
That would mean taking three of the prescription tablets daily to hit the recommended dosage (assuming the elemental iron was 60mg). Taking just one prescription tablet makes me feel terribly nauseous so I can’t imagine taking three per day!
It’s estimated that, assuming no problems with absorption, you’d need to take this much iron for four weeks to correct a moderate deficiency. If you have a severe deficiency it make take months to correct. If you have heavy periods, like me, you’d need to be on iron constantly. For someone who has to be on it long term, compliance with the prescription tablets is really hard because of all the side effects.
The good news is that there is another option.
Other forms of iron – such as carbonyl iron and iron bisglycinate – are thought to be safer, have high absorbability and cause less side effects. In my experience they work well and they are much better to take over the long term. The challenge with these supplements is that they contain less elemental iron than the prescription iron tablets. Therefore you will need to take more of them each day to restore your iron levels.
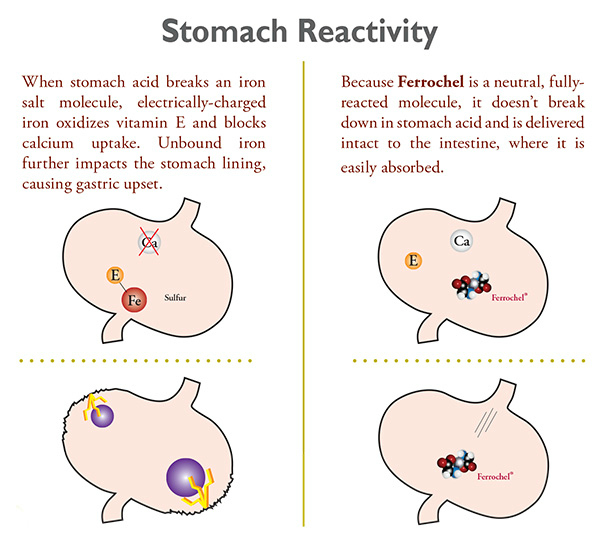
One of the most common gentler forms of iron is Ferrochel®. I’ve experimented with other forms of gentler iron and this is the one that has worked best for me and I’ve seen good results with my clients as well. You’ll find Ferrochel® in many iron supplements (I use the Blue Bonnet supplement shown in the photo above). The following is a diagram showing how Ferrochel® is easier on the stomach as compared to other supplements using iron salts.
Photo Source: Albion
I have taken up to six capsules per day after heavy periods with no stomach problems. Six per day will be about 160mg of iron so it’s getting into the range recommended by doctors to reverse iron deficiency. I usually take it in two doses about 45 minutes on an empty stomach before lunch and dinner.
The Link Between Heavy Periods and Low Iron
A heavy period is usually defined as losing more than 80 ml of blood per period. For some women a heavy period could mean as much as 1 cup of blood lost.
1 cup of blood lost is 100-125 mg of iron lost.
That’s a lot of iron! If your basic needs are already 18mg per day then you need to add an extra 25-30mg per day for at least 5 days after your period to make up the shortfall. Remember your body doesn’t absorb all the iron from food or supplements (although you do absorb more when your iron is low), so if you are trying to replenish after a heavy period you’ll need your intake to come to more than 100-125 over the following week or so plus the 18g per day for your daily needs. You can see how difficult it will be to get this from food alone.
If you don’t replace the iron lost your iron stores will keep dropping with each heavy period. This is problematic because not only do heavy period deplete iron stores but having low iron causes heavy periods. It’s a really challenging situation – especially if you are experiencing crazy 40-something periods.
The Link Between Low Iron and Thyroid
There is a link between low iron and thyroid function although more research is needed to understand this relationship. Normal thyroid function depends on the presence of many trace elements, including iodine, selenium, zinc and iron.
Studies have found that iron deficiency impairs thyroid metabolism, and that iron deficiency can cause hypothyroidism and vice versa. For example, low iron levels can increase circulating concentrations of TSH (thyroid stimulating hormone). Hypothyroidism may also lead to low iron levels due to poor gut absorption as a result of decreased levels of digestive acids/ enzymes or due to associated autoimmune conditions like celiac disease.
Iron treatment for women with subclinical hypothyroidism has been shown to create a small increase in T4 and a decrease in TSH (which is a good thing). If you are iron deficient with a thyroid condition, it’s essential that you work with your doctor to address your deficiency and see how your thyroid responds.
Final Takeaways
Making sure you absorb enough iron from your food and supplements is tricky so go back to the section on maximizing iron intake if needed and read it carefully. If your iron is really low or you struggle to get your iron back up every month after your periods, it’s important not to miss days when supplementing. Our monthly periods means there’s only a very limited amount of time for us to catch up our iron before it gets depleted again. I know how much of a struggle it can be.
For more help and advice, check out my other videos on YouTube about iron and message me in the comments there if you have questions. I hope you find some relief!